Venous Thromboembolism and Australia Pharmacy
Proven, symptomatic VTE or fatal PE occurring between discharge from hospital, when thromboprophylaxis was stopped, and 3 months later. Values in parentheses are %. 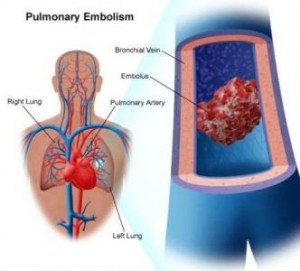
Sudden death occurred in three patients with known heart disease. No autopsies were performed, so PE was not excluded.
Thus, while extended prophylaxis appears to reduce the relative risk of symptomatic VTE by about 60%, the absolute risk reduction is low, especially for PE.
Six randomized, placebo-controlled clinical tri-als have evaluated extended LMWH prophylaxis for up to 35 days among THR patients who completed in-hospital prophylaxis with either LMWH (ie, enoxaparin or dalteparin) or warfarin. Each study observed lower rates of venographically screened DVT with extended prophylaxis. A systematic review of these six trials demonstrated a significant decrease in both total and proximal DVT with extended LMWH use, as well as reduced risk of symptomatic VTE arising during the treatment period generic viagra new zealand. The rates of out-of-hospital symptomatic VTE were 4.2% with in-hospital prophylaxis and 1.4% with extended prophylaxis (relative risk, 0.36; p < 0.001; NNT, 36). In another randomized clinical trial that compared in-hospital use of LMWH and LMWH therapy that was continued after hospital discharge, extended prophylaxis did not further prevent symptomatic VTE.
One clinical trial also confirmed the benefit of posthospital discharge pophylaxis with VKAs. More than 350 consecutive patients undergoing THR were randomized to receive warfarin prophylaxis (target INR, 2 to 3) until hospital discharge (mean duration, 9 days) or for another 4 weeks after hospital discharge. DUS was performed 1, 2, and 4 weeks post-hospital discharge. The study was prematurely terminated because of the demonstrated superiority of extended prophylaxis. VTE occurred in 5.1% of in-hospital prophylaxis patients, and in 0.5% of those who continued warfarin, a relative risk of 9.4 (95% CI, 1.2 to 73.5). The NNT to prevent one VTE using extended warfarin prophylaxis was 22.
Only one patient experienced major bleeding. In another trial of 1,279 patients undergoing THR, the LMWH reviparin (4,200 U SC once daily) was compared with a VKA (target INR, 2 to 3), both administered for 6 weeks. Objectively confirmed, symptomatic VTE occurred in 2.3% of patients receiving LMWH, and in 3.3% of those receiving the VKA (p = 0.3). However, the rates of major bleeding were 1.3% and 5.5%, respectively (p = 0.001). Thus, these studies indicate that VKAs also may provide effective extended prophylaxis after THR, although major bleeding is more frequent with the use of these anticoagulants.
Extending LMWH prophylaxis to postoperative day 28 in one clinical trial of patients undergoing TKA did not significantly reduce the rate of objectively screened DVT (17.5%) compared to 7 to 10 days of prophylaxis (20.8%). Hospital readmission rates for VTE also did not differ significantly (3.2% and 5.4%, respectively).